The gradual adoption of electronic health record systems has been in the works in more than a handful of countries around the globe, from the Kingdom of Jordan to Canada and India, all with various levels of success and interoperability. However, in the European market at least, it seems that the UK is the most proactive country in this respect, being the country with the highest uptake of EHR in the region.
A year ago, UK Health Secretary Jeremy Hunt stated that the National Health System is projected to become completely dependent on EHR within the next 5 years, a development which will allow continuity of care to become more seamless and more effective, making it possible for a physician a patient has never met before to view their complete medical history and make accurate and meaningful assessments about what the best course of action for the patient’s condition is.
For insight into just what is important to doctors when it comes to tackling the transition from paper to electronic records, Creation Healthcare conducted a mini-study of online conversations among healthcare professionals, including more than 400 tweets posted since the beginning of 2014.
One of the big questions surrounding the subject of transitioning to a completely paperless system of health records has been the extent to which patients should get access to their own medical records and what sensitive issues can arise if access is not executed in an efficient way. This issue was certainly reflected in the study data: almost 17% of healthcare professional mentions of EHR referred to studies on patient access trialling, or linked to articles and studies on the topic.
The benefits outweigh the risks, but what about the logistical challenges?
Within the study, the overall sentiment with regards to the concept of implementing electronic health records in the UK is a very positive one; however healthcare professionals have not hesitated to voice scepticism at times, as well as thinking ahead by setting a list of core principles that may be conducive to success.
One particularly popular link shared by healthcare professionals was to Cheshire-based GP Dr Amir Hannan’s story, published by blog Doctor’s Bag, a blog about “healthcare, social media and eHealth published by Dr Edwin Kruys, a GP based in Australia. The blog post tells how Dr Hannan implemented an electronic health records system allowing patients to access their records online or via a mobile device. Dr Hannan says that the approach “improves the relationship between patient and clinician, leading to a partnership of trust.”
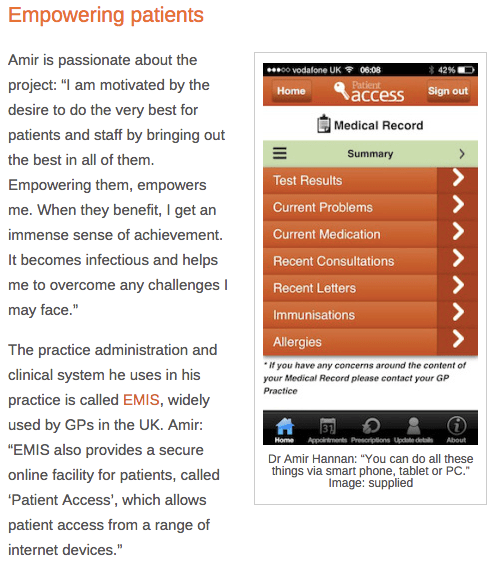
UK GP Dr Amir Hannan’s story about implementing electronic health records is shared on the Doctor’s Bag blog.
Dr Hannan’s story has been shared by some of the UK’s most prominent online healthcare professionals, including Anne-Marie Cunningham, a GP and clinical lecturer at Cardiff University, and Ash Paul , a UK-based public health doctor.
Ash Paul, a UK public health doctor, shares Dr Hannan’s story about electronic health records
It is especially interesting to note here the way the conversation is really taking place in a peer-to-peer way, from a physician publishing an interview with another healthcare professional whose activity is notable and respected, to the community of healthcare professionals promoting and sharing what they believe is a worthwhile story. This signals trust and helps disseminate knowledge and motivation around the topic of electronic health records to all online doctors or healthcare assistants interested in the subject.
In response to Dr Hannan’s story, Peter Davies, a West Midlands based physician and endocrinologist responds with a sceptical tweet, adding his own views on the subject in the form of a blog post in which he shares the story of Dr Davies’ father, who keeps a hefty paper record of all of his medical data, in the absence of other options. Davies also mentions a Midlands-based CCR (Central Care Record), but laments the fact that it is missing the ability to let patients view their own data.
“Patient access seems to be a very sensitive area for GPs in particular and I have encountered a number of patients in my area who had been given a rather hostile response when they have raised questions about access to their own records. …From next April GPs will be mandated to allow patients to make and change appointments online and be able to order repeat prescriptions, but patients will have to wait a further year to have a mandate to get electronic access their record. Until then it is possible to request a paper copy for a fee. I feel sure that patient access will be the critical factor that increases data quality over time.”
Access and Health Literacy among UK patients
Another question articulated by doctors was that of patient health literacy and numeracy, as well as how the NHS will go about collaborating with Health IT vendors.
Around 11% of mentions relating to electronic health records focused on news and developments around various health IT systems and vendors, with doctors sharing concerns about vendor reliability, ownership of health records, and software integration. London-based doctor and clinical intelligence planner Dr Saif Abed commented on the importance of collaboration with Health IT vendors: “@NHSConfed_Press @Jeremy_Hunt Will require plenty of collaboration with #EHR #HealthIT vendors to succeed.”
Dr. Abed also articulates the need for a positive user experience for all parties involved, to avoid increased administration time for clinicians.
Dr Saif Abed tweets about the need for a positive user experience for all in electronic health records.
So far we are seeing a majority of UK-based healthcare professionals who are inclined to believe that the benefits of EHR outweigh possible risks (which can be mitigated). For the time being, a major concern remains tackling provider and vendor related difficulties as well as logistical challenges at local, regional, and country level.
The NHS’s ambitious plans for digital access to health record for all aims to facilitate the NHS embracing technological revolution, to bring the system up to date in a country where most aspects of daily life are objectively considered ‘technologically advanced’.
As more and more NHS trusts and surgeries adopt and implement EHR systems and practice, we will no doubt see more conversation around the topic from UK healthcare professionals. We will continue to track success stories from practices around the country, as well as monitoring how the landscape is shifting over the year 2015.

