3 days ago, I had the privilege of attending the second day of Health 2.0 Europe in London, a conference that was packed with inspiring health start-up companies that are all pioneering new ways of improving health outcomes through the use of technology.
The day was a combination of presentations delivered by health entrepreneurs and debates where members of the medical community, be they HCPs or stakeholders affiliated with the NHS, were given a chance to weigh in and tell us how they see the future digital health in an increasingly complex and competitive market.
Health 2.0 events follow what is called a ‘live demo format’, where each of the presenters gets 4 minutes to demo their app or idea – this is followed by a Q &A session with members of the moderating panel and the public.
Technological Innovations and Pharma-Patient Collaborations
Among the examples that stood out for me was the Teddy the Guardian toy, aimed at providing paediatricians with more accurate data points whilst taking the anxiety factor out of the family’s visit to the surgery. Developed by iDerma, a med tech start up based in Croatia, the medical sensor-filled plush teddy bear is used in surgeries to provide children with a reassuring, calming activity before their visit to the doctor. Upon physical contact, the teddy bear takes the child’s vital signs, which include oxygen levels and body temperature. I chatted to Josipa Majic, founder of the start-up, and she told me that measuring oxygen levels before the child is admitted into their doctor’s office proved particularly helpful in cases of bronchitis as it eliminated the need to use devices to establish them, which parents found was a more pleasant experience for their children.

Figure 1: Teddy the Guardian readings are sent to a tablet, smartphone or web app.
Also intriguing was the Abbvie ‘Deep Dive Session’, which had the presenters talk about a case study based on an app aimed at patients with rheumatoid arthritis. The app was the result of months of collaboration between biotech company Abbvie, the Netherlands’ ‘Sense Observation Systems’ and Marieke Voshaar, a patient with Rheumatoid Arthritis (RA). The app allows patients suffering from the disease to map out different symptom patterns over time, as well as helping them identify ‘bad days’ beforehand, so they can make the necessary adjustments to avoid any disruptive situations. ‘Co-creation is the key to innovation’ seemed to be the presentation’s bottom line, a statement I agree with and that I think is often overlooked in the realm of digital health.

The rheumatoid arthritis app helps patients document their pain patterns. Source: https://twitter.com/Health2eu/status/402747481278410752/photo/1
BMJ Best Practice – Are decision-making tools for HCPs the future?
I also spoke with the team from BMJ Best Practice, a point of care tool developed to assist physicians in making decisions from diagnosis to treatment. The portal is designed to help clinicians obtain quick and easily accessible up-to-date information on a wide range of medical topics.
BestPractice is being developed by BMJ’s Evidence Centre, and its unique selling point is the fact that it combines peer-reviewed information and guidelines with the centre’s latest evidence-based research, thus eliminating the need for HCPs to consult multiple sources if they find themselves in a difficult medical scenario. The portal includes an international team of caregivers, physicians, pharmacists, nurses and pharmaceutical and medical editors.
Comprising of more than 3000 different diagnostic processes, BestPractice seems to be a comprehensive resource in terms of identifying symptoms as well as seeking treatment advice for specific patient groups. There are several types of articles available on the website, including assessments (which cover diagnostic procedures and urgent considerations) and overviews (which provide a general synopsis on a group of conditions with links to clinical evidence).
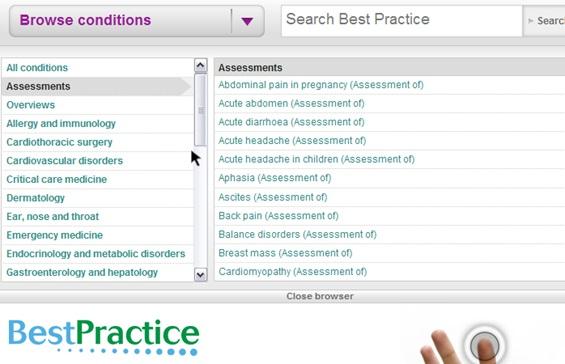
The BMJ Best Practice website – an overview of assessment type articles.
The format of the website aims to provide a fairly seamless experience as it integrates resources such as PUBMED journals, patient leaflets and allows users to click through to a topic and start discussing it on Doc2Doc , the BMJ’s forum and social network for healthcare professionals. The platform claims to be compatible to be integrated into EMR databases, and also available on mobile.
Yesterday’s event made a point of emphasising the importance of developing resources and apps in conjunction with and taking into consideration the needs and opinion of HCPs. It is often surprising that within the growing digital health landscape, quite a few companies still neglect to do this.
As a decision-making tool for clinicians, BMJ Best Practice provides a means for HCPs to seek reassurance with regards to patient safety if they are ever in doubt or faced with an atypical medical decision.
It would be interesting to see how tools like the BMJ’s BestPractice fare among other platforms of engagement and open social media initiatives such as #FOAMED, the physician-led global movement which has a significant online following and participation.
Creation.co’s previous studies into how HCPs behave online suggest the number of HCPs who regularly share information on open social media platforms such as Twitter or Google+ is on the rise.Thus, I think the BMJ providing access to decision-making tools is an important step to continuously improve health outcomes by facilitating communication among peers. However, openly and instantly requesting medical information using a well-established hashtag chat also seems to have become an established method for many online healthcare professionals, such as members of the #FOAMED movement.
What are your thoughts? How can decision making resources for HCPs complement clinical Twitter chats on social networks? How can communities of HCPs on open social media networks improve the way they communicate with each other? Is there an optimal way or organising and collecting medical resources that can be shared by doctors all over the world?
Leave us a comment, or contact us via our social networks as follows:

