Key takeaways
- The number of positive HCP online conversations about antidepressants greatly outnumber the negative conversations.
- Among the negative discourse about SSRIs (Selective Serotonin Reuptake Inhibitors), ‘side effects’ is the leading conversation topic among HCPs.
- Many HCPs in the study have their own personal experience with using antidepressants. The majority of HCPs share their experiences as well as reposting the shared experiences of other non-HCPs. Many HCPs also share posts and articles about SSRI research and trial data.
- Prozac is the most discussed SSRI, followed by Lustral.
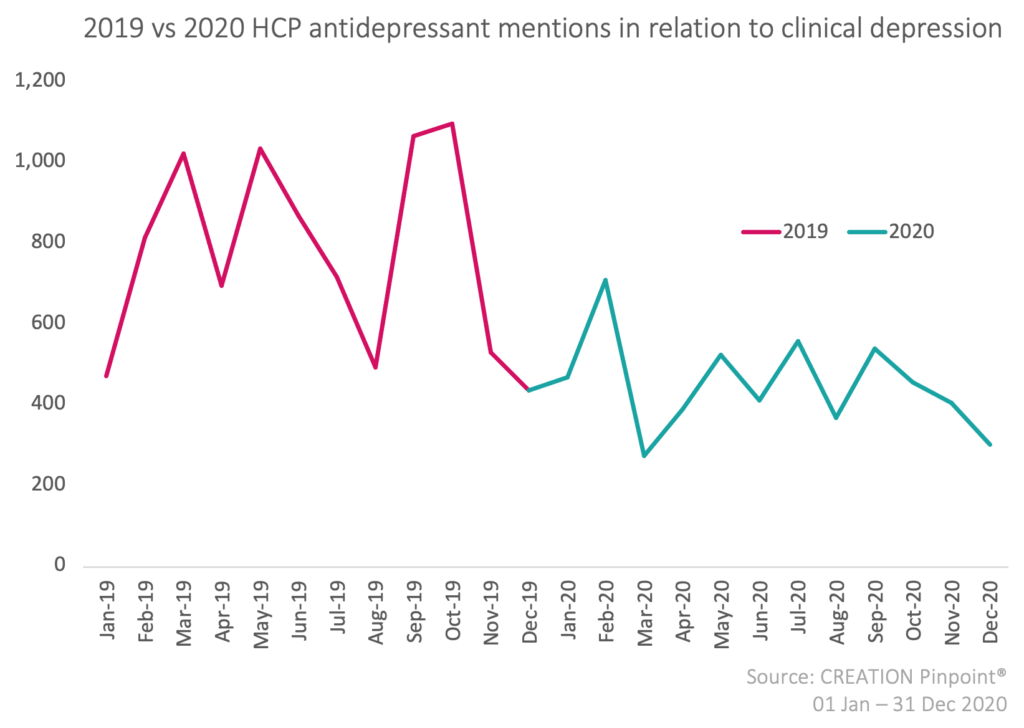
- Despite the depression rate doubling from 2019 to 2020, the online conversations among HCP about antidepressants have significantly decreased.
According to the Office of National Statistics (ONS), the number of individuals diagnosed with clinical depression doubled from 2019 to 2020 throughout the UK. Nevertheless, even with more awareness, increased diagnoses and suicide rates, the number of people receiving treatment which address both the root causes such as cognitive behavioural therapy (CBT), as well as the symptoms, such as selective serotonin reuptake inhibitor (SSRI) antidepressants, is still much lower than with physical or other non-mental illnesses.
According to Mind, approximately only 12.5% of mental health patients receive any kind of treatment at all. This brings into question the role of stigma in mental health treatment. It is therefore important to know and understand what HCPs in the UK are saying about the use of antidepressant drugs as treatment for clinical depression symptoms, in order to find new and different ways to address the challenges and disparities of clinical depression of HCPs and patients.
This research is based on the analysis of almost 2,000 UK HCPs discussing antidepressants for the use of clinical depression in over 6,000 online posts throughout 2020.
Is there any negative discourse amongst HCPs online about the use of antidepressants for clinical depression?
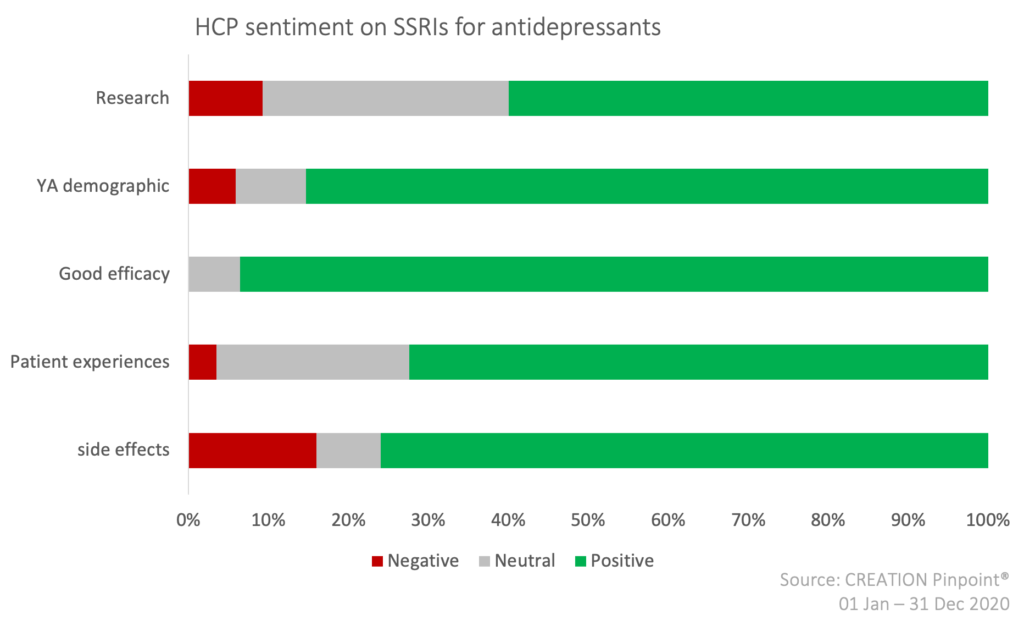
An analysis of HCP sentiment towards the use and prescription of SSRI antidepressants (Selective Serotonin Reuptake Inhibitors) in particular, indicates that the majority of HCPs speak positively or neutrally about SSRIs online.
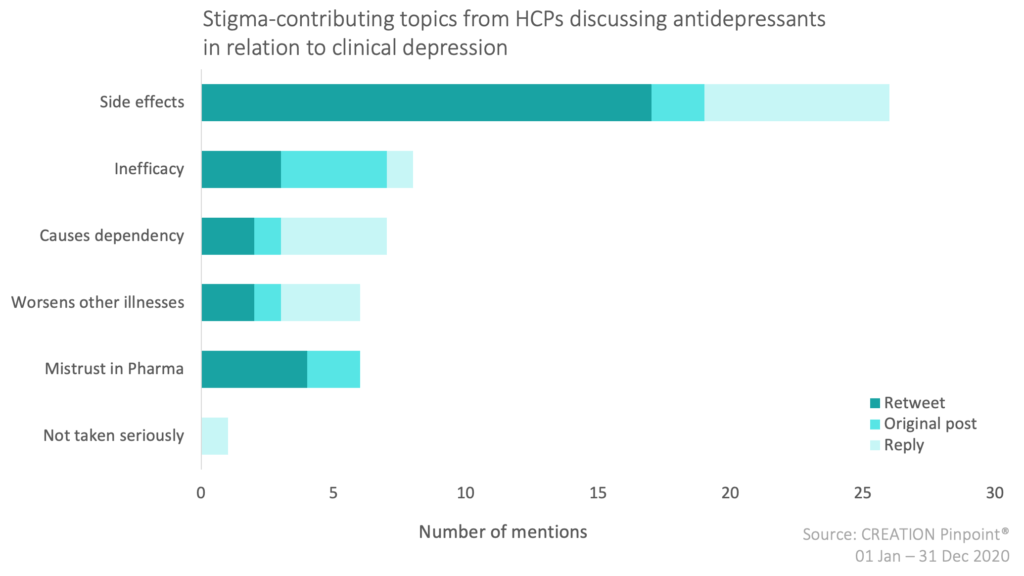
In observing the negative sentiments, we see that HCPs have expressed that the primary negative connotation associated with SSRI antidepressants is the negative side effects/adverse events. In addition, they also shared how they feel that antidepressants worsen other illnesses and cause dependency; expressing that the negatives caused by the side effects, possible worsening of other illnesses, and risk of dependency outweigh the positives. Other leading causes in the negative discourse on SSRIs are claims of inefficacy, as well as a distrust in the pharmaceutical industry among some HCPs and their patients.
We did and showed that fluoxetine associated with an increased risk of self harm in depressed CYP… increase over placebo. Doing therapy at same time appeared to reduce that increased risk of SH. Hence change to SPC/license – use CBT with fluoxetine in CYP.
— Tim Kendall CBE (@timkendall1) November 25, 2020
https://twitter.com/lozzlemcfozzle/status/1315018942197501952
HCPs most often repost patients’ experiences of side effects. The reposts about side effects are predominantly about research and studies carried out about SSRIs. Whereas the replies about side effects are mainly of HCPs sharing their own personal experiences or advice on SSRIs.
What do UK HCPs think about SSRIs?
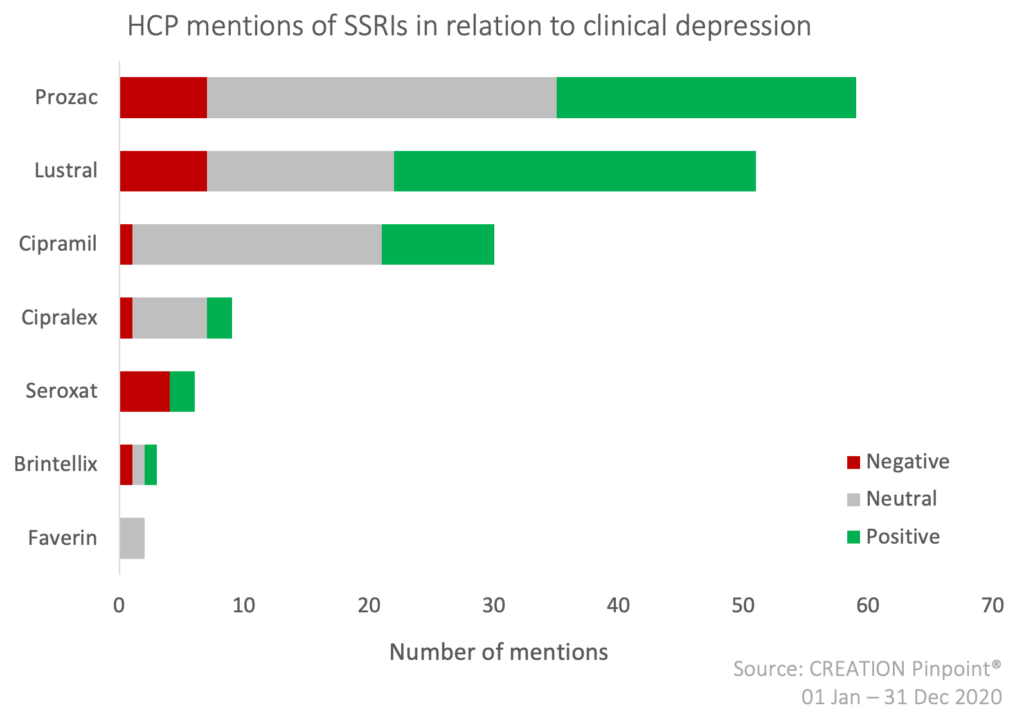
Of the 8 prescribed SSRIs in the UK, Eli Lilly’s Prozac (fluoxetine) is spoken about the most by HCPs online, followed by Pfizer’s Lustral (sertraline) and Lundbeck’s Cipramil (citalopram). The positive mentions are mostly of HCPs discussing the good efficacy of the products, and negative sentiments reflect the topics described above, such as side-effects and dependency. The positive-negative ratio indicates that most HCPs think that the good efficacy and positive aspects of the products outweigh the negative.
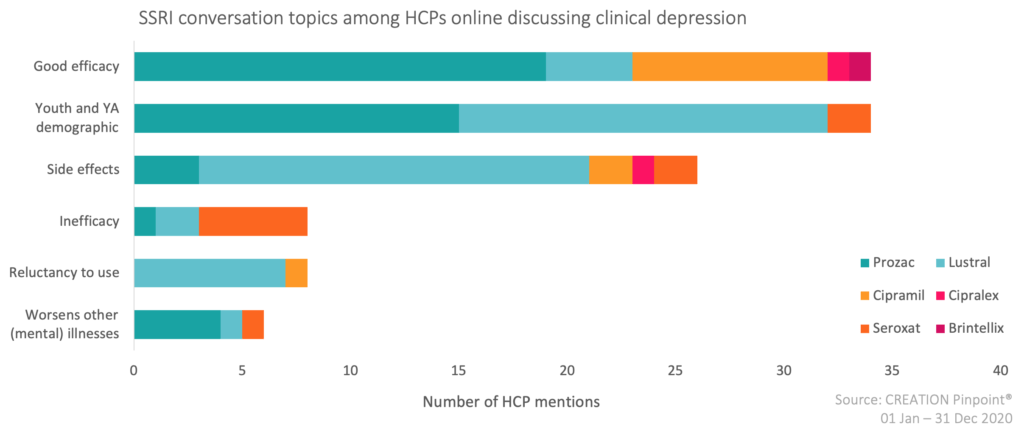
The leading SSRI conversation topics among HCPs are good efficacy and adolescent usage. Good efficacy is spoken about in regard to almost all products, but especially Prozac. Whereas inefficacy is spoken about the most in regard to GSK’s Seroxat (paroxetine), which is not included in the HCPs’ good efficacy conversation. Pfizer’s Lustral (sertraline) additionally contributes little to HCP conversations on good efficacy, yet is the main product spoken about side effects.
A small study of five female adolescents who had been on Prozac® for major depressive disorder showed a reduction in depression scores by 56% when supplemented with creatine.https://t.co/C0W4npFyj8
— Eashwarran Kohilathas (@drkohilathas) December 21, 2020
There is also much conversation specifically about the youth and young adult demographic using SSRIs, particularly when it comes to taking Lustral and Prozac, which are FDA approved for treating OCD and depression in children.
How are HCPs discussing antidepressants online?
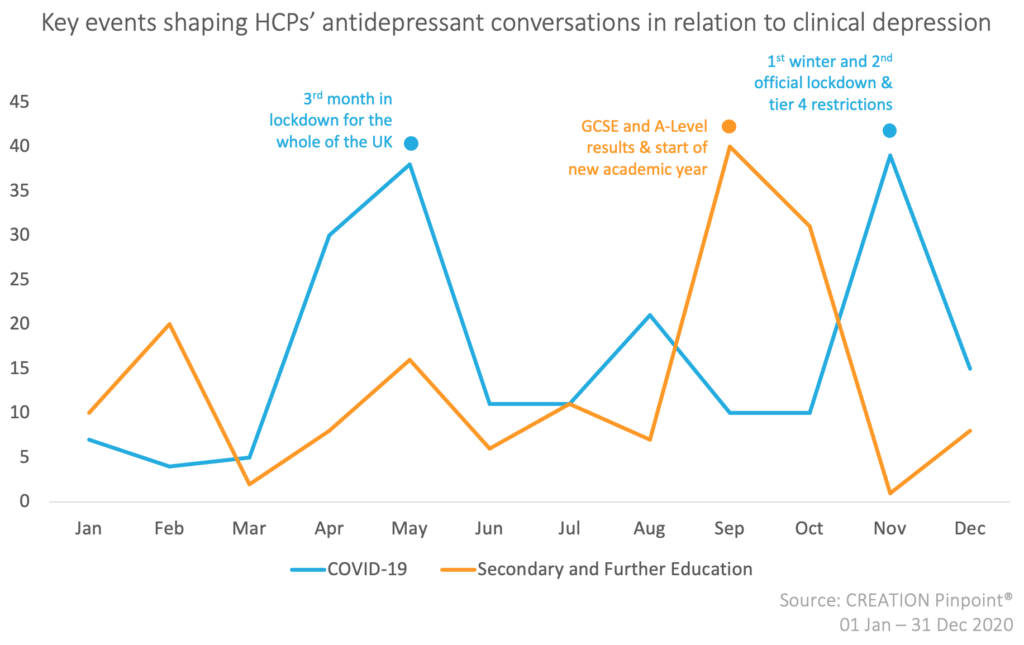
- COVID-19 and education shaped antidepressants conversations in 2020
Among the many historic and noteworthy events of 2020, the two that contributed the most to the antidepressants conversations among HCPs online were:
- COVID-19: conversations about the impact of lockdown, recessions, social distancing, and restrictions on depression and an increase in antidepressant use
- Secondary and Further Education: Conversations about A-levels and GCSE exams and results
2. HCP online conversations about antidepressants have significantly decreased from 2019 to 2020
Although depression rates doubled from 2019 to 2020, the online conversations about antidepressants among HCPs have decreased by over 58%. In 2019, antidepressants (ADs) were mentioned in over 9,200 online posts by more than 2,400 UK HCPs, whereas, in 2020, ADs were mentioned in 5,359 online posts by 1,814 UK HCPs.
For more information on what HCPs think about antidepressants, or any health topic, and how they are discussing it online with their peers and the public, get in touch, we’d love to help.



