05.03.2024 | Health Strategy
Online HCPs divided on schizophrenia causes and treatments
Towards the end of 2023, the FDA accepted a new drug application from Karuna Therapeutics, acquired by Bristol Myers Squibb (BMS), for KarXT to treat schizophrenia.
Approval is expected in late 2024 and if successful, KarXT would be the first new pharmacological approach to the treatment of schizophrenia for several decades. Various other drugs and therapies exist to support the treatment of symptoms faced by patients with schizophrenia but emerging treatments offer new hope for better health outcomes.
Listening to the voice of online HCPs helps you to understand what they care about. It highlights opportunities where you can align with and proactively support HCPs, outside of the product conversation.
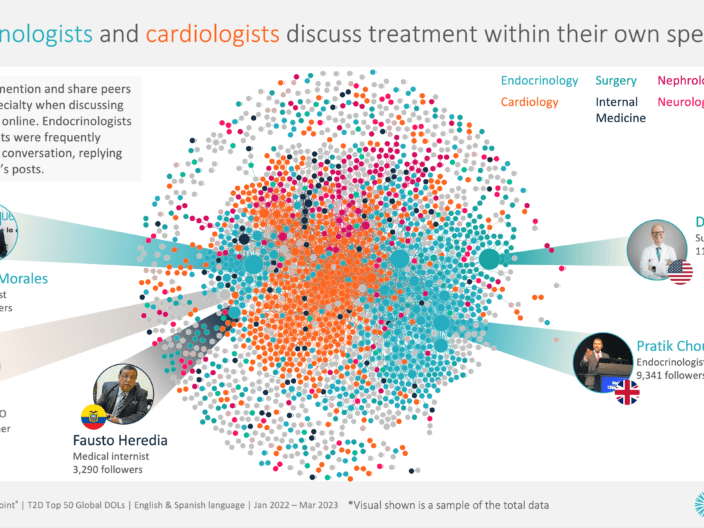
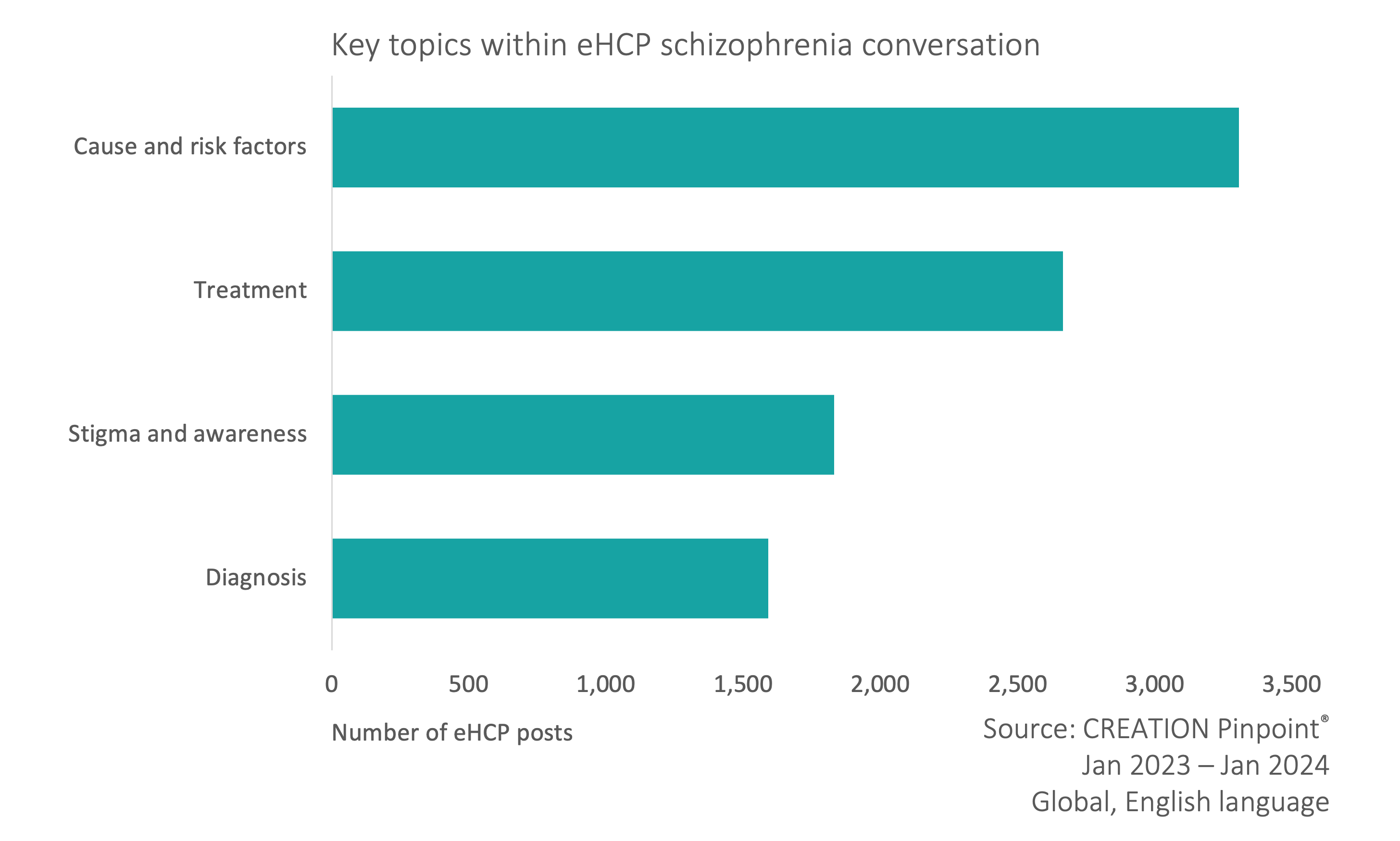
CREATION.co analysed the online English conversations of almost 5,000 eHCPs (online healthcare professionals) globally discussing schizophrenia. Four key areas emerged in the conversation with eHCPs sharing differences in opinions;
- Cause and risk factors.
- Treatment.
- Stigma and awareness.
- Diagnosis.
Cannabis: correlation vs causation
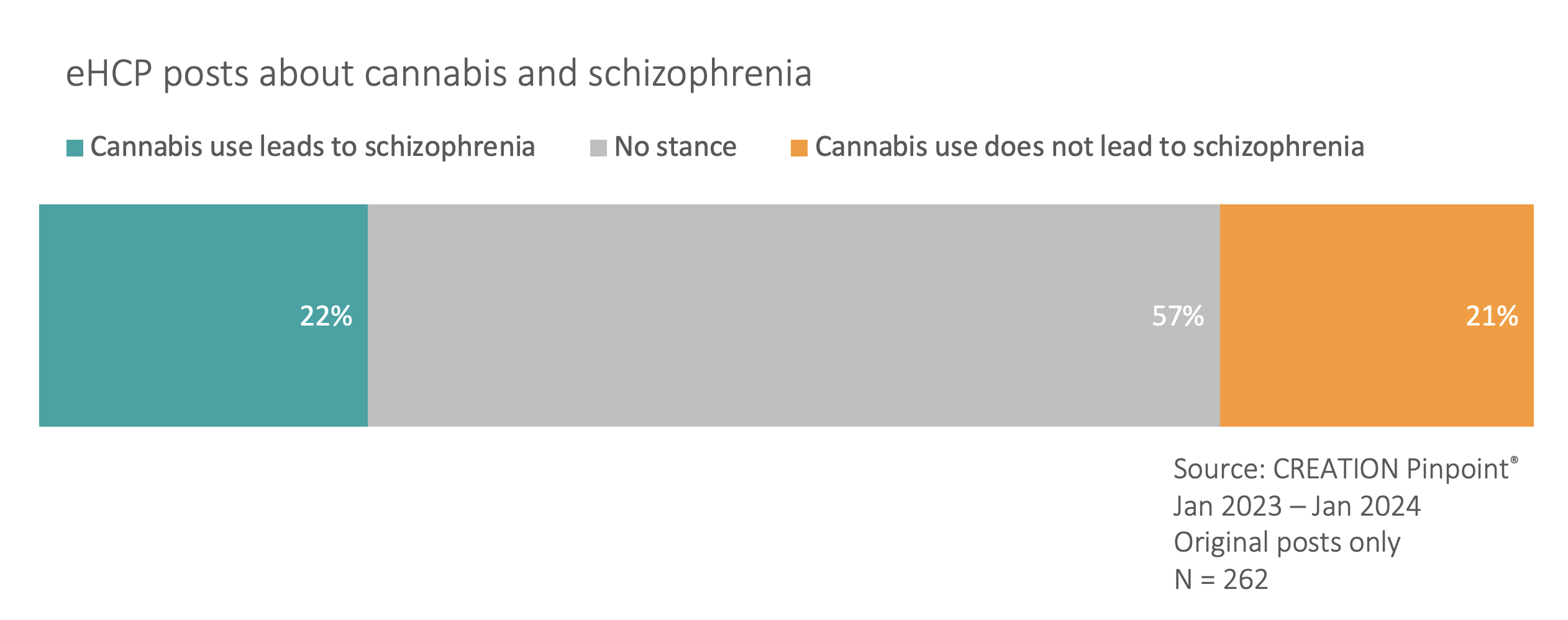
Throughout the eHCP schizophrenia conversation, there are 737 explicit mentions of cannabis (5% of posts), made up of 262 original posts and 475 shared posts. However, reviewing these posts reveals a disagreement among the HCP community of whether cannabis use is causally related to an onset of schizophrenia symptoms.
A post which received significant traction was written by Ryan Marino, an ER doctor in the US, who called out “incorrect” information shared about marijuana triggering schizophrenia episodes.
He stated that “nobody has ever shown that cannabis causes schizophrenia” and “correlation is not the same as causation”. He then argued that the effects of alcohol and tobacco cause a “magnitude” of stories.
ER doc here. This is not a controversial take; it’s an incorrect take. Nobody has ever shown that cannabis causes schizophrenia and believe me they’ve tried. Correlation is not the same as causation. I have orders of magnitude more stories about the effects of alcohol and tobacco pic.twitter.com/FM1fEF7nSO
— Ryan Marino, MD (@RyanMarino) December 12, 2023
One responder to the thread said THC and schizophrenia are a “chicken-egg situation”, explaining that cannabis is sometimes used to calm symptoms which appears to exacerbate symptoms.
On the other hand, Tyler Black, a psychiatrist in Canada, shared data from a recent study stating that “cannabis [is] highly implicated for increasing the chances of schizophrenia”, adding that more evidence is pointing towards a causal link.
Cannabis highly implicated for increasing the chances of developing schizophrenia, especially under the age of 24, whether or not that cannabis use resulted in psychotic symptoms.
More and more evidence points to cannabis as a cause; I generally recommend limiting use <24. https://t.co/B8FjxrAwXh
— Tyler Black, MD (@tylerblack32) October 3, 2023
When responders were concerned about his referral to cannabis as a cause, he simply provided a list of studies that point towards this conclusion. Doubters again pointed to cannabis simply revealing an existing and underlying problem which would reveal itself without drug use, rather than cannabis causing said symptoms.
One stance that appears to be widely accepted is that cannabis (specifically THC) is harmful to young people who are predisposed to schizophrenia. Mike Hart, a family doctor in Canada, implored parents to stop their teenagers from using it, recommending CBD to aid the THC withdrawal process.
THC is really harmful to teenagers and those predisposed to schizophrenia.
Get your teens off it ASAP.
CBD is not harmful and can benefit teens suffering from THC withdrawal.
If THC withdrawals are severe, a THC/CBD oil may help for a short-term period.
— Mike Hart, M.D (@drmikehart) May 22, 2023
On Linkedin, US psychiatrist Stefani La Frenierre, shared insights from an article exploring epigenetic changes in long-term marijuana users, with a focus on understanding this to enhance abilities to screen and intervene early.
In light of the conflicting views on the matter of correlation vs causation between cannabis use and schizophrenia symptoms, there is a need to find a consensus based on available (or future) data. Where HCPs are misaligned on this matter, there is a wealth of information being shared, without solid conclusions being made. This division impacts stigma and attitudes towards the disease from both the public and medical communities.
HCPs share views on schizophrenia treatments
Existing treatment: Clozapine
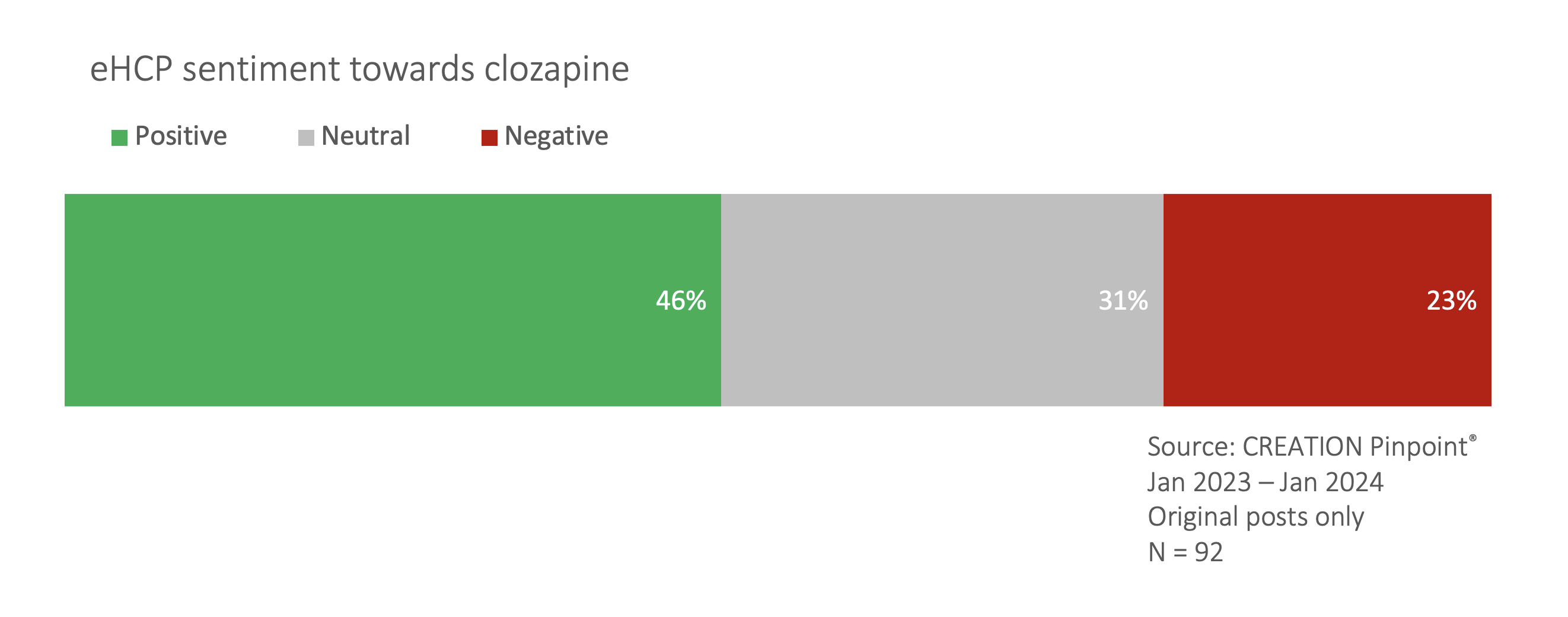
Schizophrenia can be treated with a combination of talking therapies and antipsychotics of which there are two main types. One atypical antipsychotic discussed by eHCPs was clozapine. While largely considered to be very important for the treatment of schizophrenia and a preferred treatment choice (77% of positive sentiment treatment posts), eHCPs also noted issues of side effects (70% of negative sentiment posts) and the need for close monitoring.
Clozapine is a medication which can help people suffering from schizophrenia get better when they haven’t responded to other treatments. Unfortunately, it has a range of side effects, including rarely on the immune system, & it means that people on it need close blood monitoring
— Dr Ben Spencer (@DrBenSpencer) January 17, 2024
On Linkedin, US psychiatrist Erik Messamore drew attention to the issue of clozapine access in the US, saying every other developed country has a way to get the drug to those who need it to prevent suicide in schizophrenia.
Emerging treatment: KarXT
As well as discussing established and familiar treatments, eHCPs also looked to the future. KarXT, referenced 85 times by eHCPs, recently published “impressive” phase III data showing efficacy in reducing symptoms.
Efficacy and safety of the muscarinic receptor agonist KarXT (xanomeline–trospium) in schizophrenia:https://t.co/5Rg76QZbtx
Impressive phase 3 trial showing efficacy of KarXT in reducing positive and negative symptoms pic.twitter.com/07WwN8Evyp
— Sahit Nallani Menon (@sahitmenon) January 18, 2024
US psychiatrist Mehul Mankad celebrated the trial, specifically that it did not focus on dopamine and 5HT.
Yes! Nice to see a trial that does not focus on dopamine and 5HT for treatment of schizophrenia. Why not address the ACh side of the ACh-DA see- saw?!?
KarXT reduces symptom severity in schizophrenia https://t.co/1i49sbxMje
— Mehul Mankad, M.D. (@mankadmd) June 5, 2023
Despite the optimism about this potential new option, there were hesitations. Joe Pierre, a psychiatrist in the US, said there may not be much efficacy beyond clozapine, but side effects could be a differentiator.
yes, there are certainly relevant differences wrt side effects, but not so much efficacy beyond clozapine.
the real ? is whether KarXT will be helpful for those who don't respond to other meds or whether it's novel MOA will make it more like mirtazapine (different but same).
— Joe Pierre, MD (@psychunseen) September 26, 2023
Stigma and correcting misinformation
The eHCP conversation exposes the extent of stigma faced not only by those with schizophrenia, but any psychiatric disorder. Canadian psychologist Jonathan Stea even had to defend the existence of schizophrenia and other mental illnesses, calling attention to anti-psychiatry stigma.
Schizophrenia exists.
Mental illness exists.
Psychiatric medications can be life-saving.
Psychotherapy can be life-saving.
Don't let misinformed people tell you otherwise.
Enough with the anti-psychiatry propaganda and stigma. ✌️ pic.twitter.com/9NBVUJP69t
— Dr. Jonathan N. Stea (@jonathanstea) January 6, 2024
27% of the stigma conversation happened around National Schizophrenia Awareness Day (#NSAD2023) and World Schizophrenia Day which successfully attract positive conversations about schizophrenia and generally raise awareness about the symptoms and challenges posed by the disease. Advance mental health practitioner and CEO at Rethink Mental Illness, Mark Winstanley, was vocal during #NSAD23, particularly calling for dispelling myths.
Let’s dispel the myths and challenge the stigma around schizophrenia today on National Schizophrenia Awareness Day. @Rethink_ 👇🏼 are here to help everyone better understand this most misunderstood condition. #NSAD2023 https://t.co/p1Undo87Ys
— mark winstanley (@charitablemark) July 25, 2023
One line of discourse was around stigma coming from healthcare professionals themselves and how this affects the patients experience of their own diagnosis. Psychologist and mental health advocate Dr Veenu Gupta shared research about lived experience adding that a “schizophrenia diagnosis is mostly rejected due to stigma the label invokes”.
A schizophrenia diagnosis is mostly rejected due to stigma the label invokes if it is an accurate representation of the lived experience of the patient. A redefinition of the label is not needed from psychologists that challenge its validity who have no clinical experience. https://t.co/kw1l2IDg5t
— Dr Veenu Gupta (She/Her) (@TheTealTigerUK) January 7, 2024
Stigma is also noticed in the media, where Nandini Chakraborty noted words such as “delusional” and “schizophrenic” thrown about loosely and widely.
I hear the word 'delusional' and 'schizophrenic' thrown about by the media so loosely and widely. Does not do anything for stigma and understanding a complex illness and very distressing symptomatology.
These are not words to be thrown at people who don't agree with you.— NANDINI CHAKRABORTY (@DrNandiniC) February 20, 2023
Early detection and diagnosis
It is largely true across disease areas and, according to psychiatrist Erik Messamore, the case for schizophrenia, that outcomes for patients are better with early detection and treatment. In schizophrenia, our research shows that stigma is an interfering factor to this.
In a thread on X debunking common misconceptions about schizophrenia, psychiatrist Sulman Aziz Mirza in the US said that schizophrenia is not just adult-onset and that early intervention can make all the difference for patients.
It’s Not Just Adult-Onset
Schizophrenia can start young.
• Early signs in adolescence
• Consult if behaviors change
• Timely diagnosis helps
Early intervention can make all the difference.
— Sulman Aziz Mirza, MD? | TheKicksShrink (@sulmoney) September 15, 2023
Our analysis of the eHCP conversation reveals that diagnosis of schizophrenia, let alone early diagnosis, is not straightforward. Tyler Black, an emergency psychiatrist in Canada, reminded his peers that schizophrenia cannot be diagnosed through a checklist. He followed with six routes required to make such a diagnosis. However, a psychologist, Dr Luis F. Morales Knight, responded that the DSM is full of checklists, stating that a better ruleset is needed for consistent and correct diagnosis.
A note to all researchers, scientists & clinicians:
One does NOT diagnose severe psychiatric disorders like bipolar disorder, schizophrenia, severe depression, etc. through a checklist!
(Really any psychiatric disorder for that matter)
— Tyler Black, MD (@tylerblack32) April 30, 2023
The issue of misdiagnosis arose, specifically from Chris Palmer, a psychiatrist in the US, who was alerted to psychosis symptoms as a result of B12 deficiency being misdiagnosed as schizophrenia. He mentioned that B12 deficiency in a North Indian population is at endemic rates, and speculated that many people may have been incorrectly diagnosed with schizophrenia as a result.
What causes auditory hallucinations, persecutory delusions, thought broadcasting, and insomnia?
In this case, it was vitamin B12 deficiency.
How often do we just diagnose it as schizophrenia and call it a day?#BrainEnergyhttps://t.co/xNclDiG3Tj
— Chris Palmer, MD (@ChrisPalmerMD) May 24, 2023
Unbranded communications can provide HCP support
Broadly, the eHCP conversation in schizophrenia reveals a level of discrepancy across views and understanding. Some eHCPs believe cannabis causes schizophrenia, whereas others disagree. Some look to new treatments while their peers advocate for better access to existing medications. Even attitudes towards the disease itself, sometimes contributing to widespread stigma, are inconsistent throughout the HCP community, although the majority lean towards holistically supporting patients.
Despite advancements in research and the development of new treatments, there is a need for consensus among HCPs based on available data to create unity and consistency for both those treating schizophrenia and their patients. The discussions reflect discrepancies in the understanding of and approaches to schizophrenia, indicating the need to address stigma, improve access to effective treatments and enhance diagnostic methods for better patient outcomes. These learnings from the online conversation display how pharmaceutical companies and other health stakeholders in this area can work towards better health; with better listening.
To discover how better listening will lead to better health email [email protected].
 By Mary Kangley
By Mary Kangley